Have you ever noticed that some people have irritating habits that they may not even be aware of?
Although, I give everyone the benefit of the doubt and pride myself on intent listening and critical thinking skills, I cannot help but wonder about how some people may feel defined by their chronic health conditions. Is it possible that certain habits, such as addictions, lack of exercise, poor hygiene, specific dietary patterns or excessive caffeine use, may be contributing to certain chronic health condition and if only the person was willing to change their behaviour they may be able to overcome their dis-ease? Is it also possible though that other, more subtle habits, such as negative thinking, worry or anger, among other factors might be contributing to illness? On the opposite side of the coin, I am constantly amazed by the unrelenting dedication of many people to overcome their diseases. With hard work and commitment, I have seen many “miracles ” with respect to people reversing “irreversible” conditions.
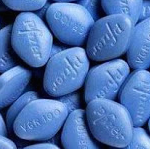
Still, it makes you wonder, when people are suffering for years with a chronic condition, such as a chronic cough, body pains, phobias, stress, depression, erectile dysfunction or even menopausal symptoms, is it not possible that they have in part habituated to their condition and partly need to work on changing the behaviours that may be contributing to their chronic illness.
Although I refuse to diagnose or label diseases because of the known psychological impact a chronic disease label can have on people, I must admit that I often rely on chronic disease diagnoses to help guide my testing recommendations and treatment options. Regardless, I wholeheartedly believe that all diseases are entirely reversible without the use of pharmaceutical medications, as outlined in the following article. So diagnosis or no diagnosis, we are aiming for the underlying cause of all chronic diseases.
As a part of my assessment I have always made a more concerted effort to try and help people better determine potential pitfalls in their lifestyles that may be contributing to chronic diseases. One recent recommendation is the Heart Rate Variability monitoring that I have been recommending to people now for several months. Although this technology has the ability to track your stress, it still relies on the person to assess the data and make sense of the stress triggers in their lives, be it food, work, or riding the bus.
At this point I need to bring up a recent case that I found interesting. A person came to me with sleep difficulties and after thorough questioning, I ran all of the testing I would typically do to assess their biochemical status and indicators of poor sleep. Sure as anything the results all came back with nothing. On further duplicate questioning however, I found out that this particular client has several glasses of wine per day, (not written on their intake form) and drinks caffeine in the afternoon. When I brought up the possibility that these lifestyle factors, along with dietary habits at night, may be contributing to the poor sleep, all heck broke loose. There was no way they were giving up their wine and caffeine to address their sleeping. They did however, try different supplements and medications (none of which I prescribed) to try to get enough sleep to function during the day.
Another interesting correlation comes to mind with respect to menopausal women. I have an 80% successful cure for hot flashes. This includes complete alcohol and caffeine elimination and 2 to 3 tablespoons of freshly ground flax seeds per day for 2 to 3 weeks. This treatment works almost every time and therefore people are willing to follow it! Despite this, I have seen many women opt into bioidentical hormone replacement therapy instead of giving up “the juice.” These things are hard to give up!
This blog was prompted after reading the following medscape article a while back on chronic throat clears. When I first read the article, I found it offensive given the “all too common” conventional down playing of peoples chronic health concerns. However, after reading the article several more time, I got to thinking that many peoples chronic health concerns can partly come from an ownership of their condition which needs to be broken!
Refractory Laryngeal Symptoms
Dr. David Johnson, Professor of Medicine and Chief of Gastroenterology at Eastern Virginia Medical School in Norfolk, Virginia.
Understanding Habituation
I want you to understand a key concept, and hopefully this will serve you well. It’s called habituation. I learned this in dealing with chronic throat clearers for a long time.
These patients come in, and I’ll be listening to them as they talk, and their symptoms are frequently a gravelly voice, voice change, or sensation in the throat. The patient will say, “Well, doc, [clears throat] um, [clears throat] um, [clears throat].”
What you pick up right away is that there is some perpetuation of a behavior here known as habituation. What we are learning is that these patients may get into a cycle that they just can’t get out of.
These patients may truly have had gastroesophageal or laryngopharyngeal reflux. As the reflux improves, the patients, however, have learned to deal with it in the way that they clear their throats or inflect their voices, and that can actually incite an ongoing inflammatory response.
Is It Repetitive Habituation-Type Behavior?
To help them understand, I use the analogy of clapping your hands together. If you clap your hands together, they get red and swollen. That is analogous to what the vocal cords are doing. I tell patients that as they clear their throats or have a dry cough or try to cough because of a sensation in their throats, it has the same effect. It perpetuates the inflammatory response.
Breaking the Cycle
After I get a good perspective that this sounds like repetitive habituation-type behavior, I talk with the patients about that and then look at a variety of things that they can do to help themselves.
One thing I insist on is having them carry a bottle of water, and every time they feel that sensation of thick secretions or a swelling-type feeling in the back of their throats, they take water rather than trying to clear it with phonation. If they have to clear it, I ask them to clear it without phonating. They should try to clear their throats softly, rather than harshly, and try to minimize the number of attempts to clear it.
Make sure that patients understand that this is going to be a process, and it’s an education. They need to recognize that they need to throttle back on using their voices if they find that their voices start to become hoarse or tired. They need to cut back on their telephone calls, yelling and screaming at games or parties, or whatever they do to overuse their voices. In social situations, they need to use their quiet voices, rather than projecting their voices, to get the inflammatory response under control.
If the patient can’t carry a bottle of water, I recommend carrying lemon drops, which help the parotid salivary secretions to flow more easily. When they are out and about, these are things they can carry with them. Emphasize hydration, and tell patients to minimize substances that dehydrate them such as caffeine and alcohol. If these patients are smokers, try to get them to stop smoking.
Voice Retraining
I have also found it very helpful to engage with a voice specialist—a physical therapist who is uniquely trained in voice. This is not just a standard speech rehabilitation specialist. It has to be somebody who understands the complexity of voice retraining. They use phonation and exercises to help with pitch and expressions, and they get the patient back down to a more restful voice.