Dysbiosis (also called dysbacteriosis) is a term used to describe the imbalance of the microbial inhabitants of the body. As this is thought to be a major contributing factor to virtually all health concerns (yes … all, even cancers), I would say that it is a pretty big deal! In my practice I see a lot of functional gastrointestinal conditions such as achalasia, gastroesophageal reflux disease, gastroparesis, delayed motility in the small intestine along with irritable bowel syndrome and most of these conditions, (but not all) are associated with microbial imbalances of the digestive system.
The concern with many functional gastrointestinal disorders, and their underlying causes, is that they are typically only the first sign of disease to arise in an individual and conventional medicine still fails to effectively identify or even recognize these concerns. One of the reasons for conventional failures in identifying and treating the cause of most functional gastrointestinal disorders, (which I have mentioned in posts before), is the failure to adopt technology that can better asses the understood causes of these disorders. The reality is that the technology has existed for decades and some of this technology is very reliable at assessing the causes of certain disorders associated with dysbiosis. These include lactulose breath testing for SIBO and “shotgun” DNA sequencing of the microbiome. Even less “accurate” testing like RNA 16s sequencing techniques that are more widely used commercially, can still provide a patient with incredible insight into the imbalance of their microbiome along with options for correcting that imbalance.
There also seems to be limited awareness in mainstream medicine about the association of dysbiosis with other health disorders despite literature on this subject dating back to the 50s. Although dybiosis and lipopolysaccharide (LPS) endotoxemia has been connected to virtually all chronic health conditions, I would like to use the autoimmune diseases Crohns and Ulcerative Colitis as brief examples because of the devastating effects that these conditions can have in the people that suffer with them. Very often, sufferers are told that these conditions have nothing to do with the food that they eat or the balance of microbes in their digestive tract. They are told, “no, its just your immune system attacking your body for no reason” …. Um, really? There is no better example of serious medical conditions that are caused by food choices and the microbiome than Crohns and Colitis …. just use logic. What is true however is that it would be very hard to prove a single cause in individual patients that suffer with these conditions, and through acceptable research to the medical profession “prove” causation. This is fortunate for the drug companies but doesn’t excuse the medical profession from not encouraging sufferers to work on the problem on their own with simple dietary advice and perhaps “direct to consumer” stool testing like Viome, DayTwo or even Aperiomics.
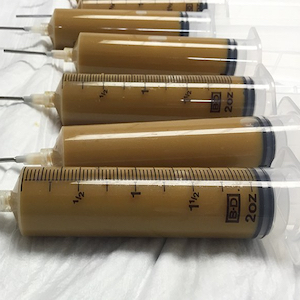
FMT or Faecal Micobiata Transplantation is always another option! FMT is a procedure that has been around for a few decades now, and is actually performed in our medical system for people with antibiotic resistant Clostridium Difficile. A medical researcher from the University of Calgary actually did a lot of early research on FMT, and started a private clinic in Calgary a decade ago that I was told was shut down by Health Canada. This treatment is actually very inexpensive to perform, as one can image, because the substrate used is literally shit! The substrate is solubilized with distilled water to a syringe-able consistency and administered it into the patient. It’s really that easy.
The following new study shows the efficacy of FMT in IBS to be an astounding 89.1%. FMT is available commercially again in Canada at the Taymount Clinic in Duncan BC. Apparently the founder, whom is a medical doctor was treated and cured of Multiple Sclerosis with FMT treatment at the original Taymount Clinic in England and pushed to set up the satellite clinic on Vancouver Island. Taymount Canada has a 10 day FMT program that starts at $10000 (or more) plus accommodations. Although it is expensive, if you are interested in FMT and faint at heart, I would advise looking into option, as Taymount uses world class poo and takes care of all the dirty work. It may sound like I’m kidding but I’m not! This also sounds like something perfect for the DIYer as a weekend project, but you are best to consult with a knowledgable medical practitioner prior to trying this at home! Anyways, have a read through the abstract of this article at the following link.
El-Salhy M, Hatlebakk JG, Gilja OH, et al. Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut. 2019 Dec 18. pii: gutjnl-2019-319630. doi: 10.1136/gutjnl-2019-319630. (Original study)
OBJECTIVE: Faecal microbiota transplantation (FMT) from healthy donors to patients with irritable bowel syndrome (IBS) has been attempted in two previous double-blind, placebo-controlled studies. While one of those studies found improvement of the IBS symptoms, the other found no effect. The present study was conducted to clarify these contradictory findings.
DESIGN: This randomised, double-blind, placebo-controlled study randomised 165 patients with IBS to placebo (own faeces), 30 g FMT or 60 g FMT at a ratio of 1:1:1. The material for FMT was obtained from one healthy, well-characterised donor, frozen and administered via gastroscope. The primary outcome was a reduction in the IBS symptoms at 3 months after FMT (response). A response was defined as a decrease of 50 or more points in the total IBS symptom score. The secondary outcome was a reduction in the dysbiosis index (DI) and a change in the intestinal bacterial profile, analysed by 16S rRNA gene sequencing, at 1 month following FMT.
RESULTS: Responses occurred in 23.6%, 76.9% (p<0.0001) and 89.1% (p<00.0001) of the patients who received placebo, 30 g FMT and 60 g FMT, respectively. These were accompanied by significant improvements in fatigue and the quality of life in patients who received FMT. The intestinal bacterial profiles changed also significantly in the groups received FMT. The FMT adverse events were mild self-limiting gastrointestinal symptoms.
CONCLUSIONS: FMT is an effective treatment for patients with IBS. Utilising a well-defined donor with a normal DI and favourable specific microbial signature is essential for successful FMT. The response to FMT increases with the dose. Trial registration www.clinicaltrials.gov (NCT03822299) and www.cristin.no (ID657402).